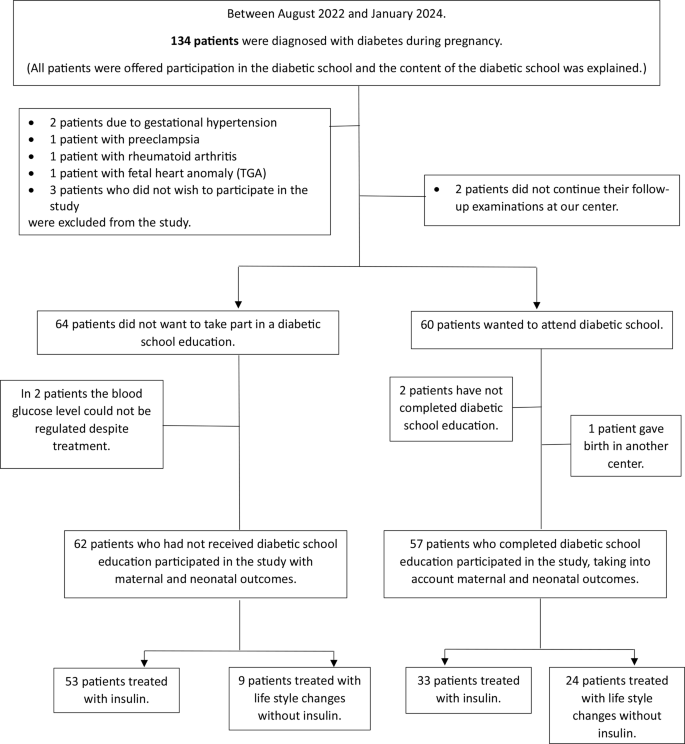
This case-control study included 119 pregnant women who gave birth in a tertiary care center between August 2022 and January 2024.
The participants were divided into two groups: The case group consisted of 57 pregnant women who were diagnosed with gestational diabetes mellitus (GDM) and referred to a diabetic school education program, while the control group consisted of 62 pregnant women who were diagnosed with GDM and did not participate in a diabetic school education program. (Fig. 1) Patients who were diagnosed with diabetes between 24 and 26 weeks of gestation with a 75 gram oral glucose tolerance test (OGTT) at a tertiary care teaching and research hospital were included in the study. Screening and diagnosis of GDM was performed with a 75 gram OGTT between 24 and 26 weeks of gestation according to the International Diabetes in Pregnancy Study Groups (IADPSG) guidelines. Gestational diabetes was diagnosed if at least one value of the 75 g OGTT was positive: fasting plasma glucose level ≥ 92 mg/dl (5.1 mmol/L) and/or 1-hour glucose level ≥ 180 mg/dl (10.0 mmol/L) and/or 2-hour glucose level ≥ 153 mg/dl (8.5 mmol/L) [15].
Inclusion criteria
Pregnant women diagnosed with gestational diabetes with a 75 g OGTT between 24 and 26 weeks of pregnancy.
Willing and able to provide informed consent for participation in the study.
Between 18 and 45 years of age.
Exclusion criteria
Who did not wish to be included in the study.
Who were unable to achieve glycemic control despite all appropriate treatment options.
Who started and then discontinued diabetic school education.
Who did not continue their prenatal care at our center.
Who gave birth at another center.
Women with multiple pregnancies, known diabetes mellitus (DM) type 1 or type 2, essential hypertension or hypertension during pregnancy, maternal nutritional disorders, liver or kidney disease, and fetal structural or cytogenetic abnormalities.
Known impaired glucose tolerance, polycystic ovary syndrome, maternal cardiovascular disease, and acontosis nigricans symptoms.
Blinding
The staff who educate patients in diabetic school education (perinatologist, endocrinologist, dietitian, diabetic nurse, etc.) are different from the staff who monitor pregnancy and make medical decisions about patients. The staff who make medical decisions about the patients and monitor the pregnancy do not know whether the patient has taken part in diabetic training. It was therefore be ensured that the monitoring of the pregnancy, the medical decisions, and the information processes in the outpatient clinic do not differ from those for patients who have not taken part in diabetic schol education.
Education and information about GDM for all patients diagnosed with GDM (control group)
Each patient in this group who was diagnosed with an OGTT of 75 g between 24 and 26 weeks of gestation was followed up according to the Turkish Ministry of Health guidelines for high-risk pregnancies at the time of diagnosis. (Supplementary Data 1) [16]. Patients were informed and given recommendations based on ACOG Practice Bulletin No. 190 (17). The content of this information includes the definition of the disease, risk factors, treatment options, follow-up protocol, complications that may occur with and without treatment, delivery management and timing of delivery, complications that may occur in the baby after delivery, and post-delivery follow-up protocol. The information ends with answers to the patient’s questions. (The longest briefing lasted a maximum of 20 min.) The patient was simultaneously examined and followed up by an endocrinologist at the time of diagnosis. The examination intervals of the endocrinologist were a maximum of 1 month. After the diagnosis of gestational diabetes, the examination interval with the perinatologist was a maximum of 2 weeks. At each outpatient visit, the patient’s health status and blood glucose level were checked by both the perinatologist and the endocrinologist [for patients treated with insulin, 7 times daily (4 fasting, 3 postprandial); for patients not treated with insulin, blood glucose levels at least twice daily (1 fasting, 1 postprandial)]. At each outpatient visit, the need for insulin treatment and, if insulin was used, the adequacy of the current treatment dose was assessed by the perinatologist or endocrinologist, and the necessary precautions were taken. In addition to the information provided by the endocrinologist and perinatologist, the diabetic nurse checked the patients’ blood pressure and weight before each outpatient examination. The patients’ questions were answered. When GDM was first diagnosed and abnormalities in blood glucose regulation were detected during prenatal care, a meeting with a nutritionist was organized under outpatient conditions. Education on the use of insulin (Supplementary Data 2) was repeated for GDM patients who required insulin treatment.
Educational program for patients attending diabetic school (case group)
This educational program was developed to supplement the education and information provided to every patient diagnosed with GDM. The diabetic training is carried out by 3 specialists, a diabetic nurse and a dietician. Each patient participating in this training is older than 24 weeks gestation and must complete the training program within 2 weeks. Each session of the training program, which consists of a total of five sessions, lasts at least 45 min. The comprehensive training content (Supplementary Data 3) includes the definition of GDM, risk factors, diagnostic methods, maternal, fetal-neonatal complications that can occur in treated and untreated patients, treatment strategies, dietary recommendations, exercise methods, and psychosocial topics.
Maternal age, gestational age, parity, body mass index at delivery, total weight gain during pregnancy, HbA1c level at presentation for delivery, method of delivery, and gestational age at delivery were recorded. Various neonatal outcomes, including preterm birth (< 37 weeks), birth weight (grams), neonatal hypoglycemia, need for phototherapy, APGAR scores at 1 and 5 min, neonatal respiratory distress syndrome (RDS), and admission to the intensive care unit were evaluated.
The difference between the groups was that, unlike the routine follow-up of pregnant women diagnosed with GDM, the patients were offered a standardized education program as part of the diabetic education program. In this program, the information to be given to the patients was more detailed, and no topics were omitted. It was not left to the clinician’s information initiative and information content. In the control group, routine follow-up care was provided, but these patients did not participate in the diabetes school education program, although they were encouraged to do so.
Statistical analysis
Statistical analyzes were performed using Jamovi, an open source statistical software, to analyze the data. The normality of the variables was analyzed using both visual methods (histograms, probability plots) and statistical tests (Kolmogorov-Smirnov/Shapiro-Wilk tests). The Levene test was used to assess the homogeneity of variances. For descriptive statistics, means and standard deviations were reported for variables with normal distribution. Group comparisons for normally distributed variables were performed using t-tests for independent samples. For non-normally distributed numerical data, medians and interquartile ranges (Q1-Q3) were used in the descriptive analysis, and the Mann-Whitney U test was used to compare groups. Categorical variables were described using frequencies and percentages, with associations between them assessed by chi-square tests or Fisher’s exact test when chi-square assumptions were violated due to low expected values. A p-value of less than 0.05 was considered statistically significant.











